

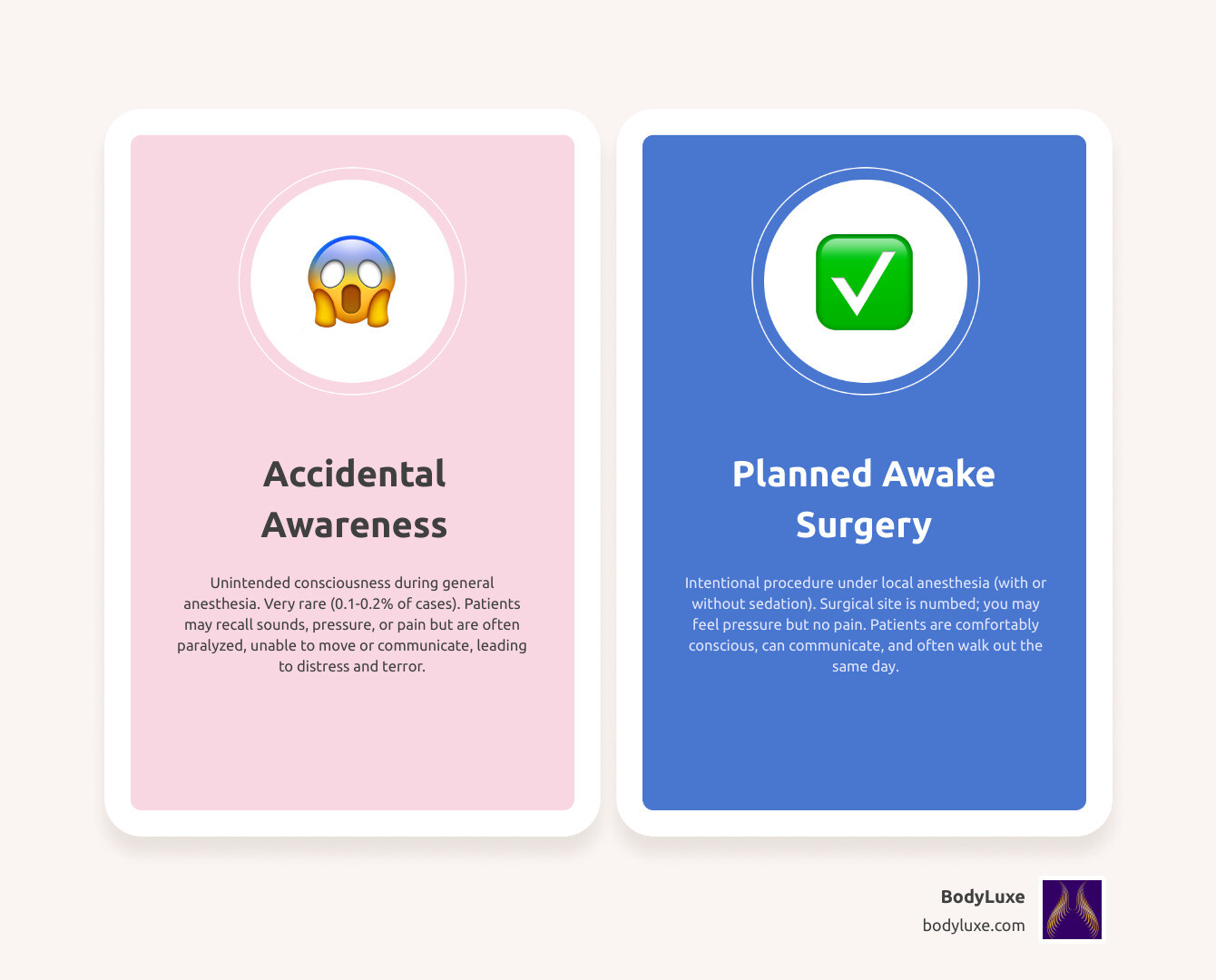
The phrase awake in surgery can mean two very different things. For many, it triggers a fear of waking up paralyzed during an operation—a nightmare scenario called anesthesia awareness, which is exceptionally rare. But there’s another kind of awake surgery that’s entirely planned, safe, and increasingly common: procedures performed under local anesthesia where you’re conscious by design.
| Type | What It Is | How Common | Patient Experience |
|---|---|---|---|
| Accidental Awareness | Unintended consciousness during general anesthesia | 1-2 in 1,000 cases (0.1-0.2%) | May recall sounds, pressure, or rarely pain; unable to move or communicate |
| Planned Awake Surgery | Intentional procedure under local anesthesia with or without sedation | Common for many procedures | Numb at surgical site, may feel pressure or vibrationbut no pain, can communicate with team |
The difference is control. Accidental awareness is a failure of general anesthesia. Planned awake surgery uses local numbing so you’re comfortably conscious, able to talk to your surgeon, and can often walk out the same day.
This guide explains both experiences, their causes, and the safety measures in modern medicine. Whether you’re worried about general anesthesia or curious about planned awake procedures, you’ll find clear answers here.
As Daniel J Farrugia MD PhD FACS, a board-certified surgeon who has performed thousands of awake in surgery body-contouring procedures at BodyLuxe in Chicago, I know that understanding this distinction helps patients make confident decisions. We’ll break down the science and safety measures that make modern surgery safer than ever.
Let’s address the fear of being awake in surgery when you’re supposed to be unconscious. This scenario is called Accidental Awareness During General Anesthesia (AAGA). It’s when you regain some level of consciousness during a procedure performed under general anesthesia.
What makes AAGA so frightening is that patients are often paralyzed by muscle relaxants. You can’t move, open your eyes, or make a sound, even if you’re aware of what’s happening. This feeling of being trapped is what makes a medical complication a terrifying experience.
What do people remember? Experiences vary. Some patients report hearing conversations or the sounds of instruments. Others recall pressure or tugging. In the most distressing cases, patients feel pain. The combination of awareness, paralysis, and sometimes pain creates an overwhelming sense of helplessness.
The psychological fallout from AAGA can be severe. About 40% of people who experience it suffer from conditions like Post-Traumatic Stress Disorder (PTSD), chronic anxiety, recurring nightmares, and depression, often requiring professional treatment to process the trauma.
Here’s the good news: AAGA is exceptionally rare. The accepted incidence is about 1 to 2 out of every 1,000 procedures involving general anesthesia—that’s less than 0.2% of all surgeries. Some studies report even lower numbers. The American Society of Anesthesiologists provides detailed statistics confirming how uncommon this is.
For over 99.8% of patients, general anesthesia works exactly as intended. You go to sleep, stay asleep, and wake up with no memory of the procedure.
However, the risk isn’t the same for everyone. Certain procedures carry a higher risk because anesthesiologists must use lighter sedation to keep the patient stable. These include:
AAGA occurs when there’s a mismatch between the anesthetic a patient receives and what they need. Several factors can cause this.
Consciousness during surgery isn’t just “on” or “off.” There’s a spectrum of sedation levels, each calibrated for different procedures. The American Society of Anesthesiologists (ASA) defines this continuum, from minimal sedation to general anesthesia. Understanding this spectrum helps explain why some procedures are intentionally performed while you’re awake and comfortable.
| Feature | General Anesthesia | Local Anesthesia with Sedation (e.g., “Twilight”) |
|---|---|---|
| Consciousness | Unconscious, unaware | Conscious but deeply relaxed, often amnesic |
| Pain Sensation | None | None at surgical site; may feel pressure |
| Breathing | Often requires assistance (breathing tube) | Independent, spontaneous breathing |
| Response to Stimuli | Unresponsive, no reflexes | Responds to verbal commands or gentle stimulation |
| Memory | No memory of procedure | Often no memory (amnesia) due to sedative effects |
| Recovery | Slower, more side effects (nausea, grogginess) | Faster, fewer side effects |
| Risk of Awareness | Accidental awareness is rare (unintended) | Planned awareness (intended) |
At the lighter end, minimal sedation (anxiolysis) calms anxiety while you remain fully awake and responsive.
Moderate sedation, or “twilight sedation,” takes you a step deeper. You’re conscious and can respond to commands but feel deeply relaxed and drowsy. A key feature is “anterograde amnesia”—many patients don’t form memories of the procedure, even though they were awake. You continue breathing on your own, a major safety advantage. This level is common for procedures like colonoscopies and is often used at BodyLuxe for our awake body contouring procedures.
Deep sedation puts you in a state where you’re not easily aroused and may need breathing assistance. It’s a step just below full unconsciousness.
General anesthesia is the deepest level—a medically induced, reversible coma. The goals are complete loss of consciousness, no pain, and no memory of the procedure. Your body’s automatic functions, like breathing, are managed by an anesthesia care team. The process involves three phases: induction (drifting off to sleep), maintenance (staying unconscious during surgery), and recovery (waking up). You can learn more about the three stages of general anesthesia from the National Institutes of Health.
While essential for many complex surgeries, general anesthesia has risks and side effects. For elective cosmetic procedures, many patients prefer the awake in surgery approach with local anesthesia and light sedation for a faster recovery and fewer side effects.

This is where being awake in surgery shifts from a fear to a smart, intentional choice. Planned awake procedures use local anesthesia to numb a specific area or regional anesthesia for larger regions. This is often combined with light sedation (a “twilight” state) so you’re relaxed but breathing on your own and able to respond.
At BodyLuxe, we use the tumescent technique. This involves injecting a dilute local anesthetic solution into the fatty tissue. This solution numbs the area, constricts blood vessels to minimize bleeding, and makes fat easier to remove smoothly. This technique has revolutionized body contouring, allowing us to perform extensive procedures like FormSculpt® Lipo while our Chicago patients are comfortably awake.
The benefits of being awake are significant. You avoid the risks of general anesthesia, such as blood clots and breathing complications. Your recovery is faster and you’ll experience less nausea. Perhaps most importantly, being awake allows for patient feedback. In cosmetic surgery, this real-time communication helps your surgeon refine the results, creating a partnership that’s impossible when you’re unconscious.
Most patients are pleasantly surprised by how calm the experience is. The surgical site will be completely numb. You will feel pressure or movement, but no sharp pain. Thanks to sedation, you’ll be in a calm and relaxed state, often drifting in and out of a light doze. Time tends to pass quickly. Throughout the procedure, communication with the surgical team remains open. If you feel anything or need to adjust, you can simply speak up. We also have nitrous gas (or laughing gas) as an optional addon to awake procedures.
The range of surgeries performed while patients are awake in surgery is expanding.
Whether you’re intentionally awake in surgery or under general anesthesia, your safety is paramount. At BodyLuxe, we believe safety relies on careful preparation, constant monitoring, and open communication.
This starts with your pre-operative consultation. We need your complete medical history, including previous anesthesia experiences, all medications and supplements, and any history of alcohol or drug use. This isn’t judgment; it’s crucial information that helps us tailor the safest anesthetic plan for your unique physiology.
For procedures under general anesthesia, preventing accidental awareness involves multiple safeguards:
For planned awake in surgery procedures at BodyLuxe, our focus is on your comfort. We use the tumescent technique to profoundly numb the surgical area. The light sedation we add keeps you relaxed while allowing you to breathe on your own and communicate with us. You are always in control.
If you believe you experienced accidental awareness during a procedure under general anesthesia, speak up. Tell your surgeon or anesthesia provider as soon as possible. Your concerns are valid and will be taken seriously.
Providers may use a structured set of questions, like the Brice Interview, to understand your experience. Write down everything you remember—sounds, sensations, feelings—while it’s fresh. If the experience was distressing, seeking psychological support is important. Accidental awareness can lead to anxiety or PTSD, and counseling can help you process the trauma and heal.
It’s exceptionally rare. Accidental awareness during general anesthesia occurs in about 1 to 2 out of every 1,000 procedures (less than 0.2%). For the vast majority of patients (over 99.8%), general anesthesia works exactly as intended, and you remain completely unconscious. Advanced monitoring and safety protocols make the risk for most routine surgeries extremely low.
No, you will not feel pain. For planned awake in surgery procedures like those at BodyLuxe, we use an advanced tumescent local anesthesia technique to completely numb the surgical area. You may feel pressure or movement, but not the sharp sensation of pain. We also use light sedation to keep you calm and relaxed. If you feel any discomfort, you can tell your surgical team immediately, and we will address it. We also can make nitrous gas (laughing gas) available to you to maintain your comfort.
For the rare individuals who experience a distressing awareness episode (especially involving pain or paralysis), the long-term psychological effects can be significant, including anxiety, nightmares, or Post-Traumatic Stress Disorder (PTSD). Professional counseling is often recommended to help process the trauma. However, brief awareness without distress typically does not result in lasting psychological harm. Choosing a planned awake in surgery procedure with local anesthesia eliminates this risk entirely.
We hope this guide has provided clarity and reassurance about being awake in surgery. Whether you’re considering a planned awake procedure or concerned about general anesthesia, knowledge is power.
To summarize, accidental awareness during general anesthesia is extraordinarily rare. Modern monitoring and protocols have made surgery safer than ever, and you can feel confident that general anesthesia is effective for the overwhelming majority of patients.
Conversely, planned awake surgery is a modern, thoughtful approach that prioritizes safety and comfort. By choosing a procedure under local anesthesia with light sedation—like the awake liposuction and BBL procedures we specialize in at BodyLuxe—you opt for a technique with a faster recovery, fewer side effects, and no risk of accidental awareness.
Your voice matters. Before any surgery, talk openly with your team. Share your history, ask questions, and voice your concerns. This conversation is the foundation for a safe experience.
Choosing the right surgeon and facility is your most important decision. Look for board-certified specialists with experience in your desired procedure. At BodyLuxe, our Chicago team is led by board-certified surgeons who have performed thousands of awake body contouring procedures using advanced tumescent local anesthesia. We are a boutique practice focused on patient education, safety, and natural, proportionate results—snatched but believable.
If you’re considering body contouring and the idea of being awake in surgery appeals to you, we’d love to help you explore your options.
Schedule your consultation with BodyLuxe today. Let’s talk about how we can help you achieve the body you want, safely and comfortably.
Back to teaching Zumba in less than 2 weeks 🙌
Awake body contouring designed to fit real life.
Natural shape. Faster recovery. Surgeon-led care.
Thank you for sharing your experience, Marisol.
“La mejor experiencia que he tenido de verdad que fue un excelente trabajo y mi recuperación en menos de dos semanas yo ya estaba dando clases de zumba me encantó la silueta que me quedó Gracias doctor Daniel J Farrugia MD PhD”
📍Chicago | Complimentary consultations available
Back to teaching Zumba in less than 2 weeks 🙌
Awake body contouring designed to fit real life.
Natural shape. Faster recovery. Surgeon-led care.
Thank you for sharing your experience, Marisol.
“La mejor experiencia que he tenido de verdad que fue un excelente trabajo y mi recuperación en menos de dos semanas yo ya estaba dando clases de zumba me encantó la silueta que me quedó Gracias doctor Daniel J Farrugia MD PhD”
📍Chicago | Complimentary consultations available
...
✨Only 3 Months Post-Op — And the Waist Is Already Undeniable.✨
This lovely patient is just 3 months post-procedure and her results are already turning heads — with final outcomes continuing to refine through 6 months.
💎 What was treated:
• Upper abdomen
• Lower abdomen
• Waist
• Flanks
• Lower back
🔥 Why this result hits different:
• Waist = snatched, sculpted, and defined
• Abdomen looks smoother and more contoured
• Back curves now flow seamlessly into the waist
• Natural shape enhancement — not overdone, just refined
💤 Procedure highlights:
• Performed awake
• No general anesthesia
• No scars, no stitches
• Recovery is typically 4–5 days
#snatched #drsnatched #bodyluxe #FormSculpt #fatremoval
✨Only 3 Months Post-Op — And the Waist Is Already Undeniable.✨
This lovely patient is just 3 months post-procedure and her results are already turning heads — with final outcomes continuing to refine through 6 months.
💎 What was treated:
• Upper abdomen
• Lower abdomen
• Waist
• Flanks
• Lower back
🔥 Why this result hits different:
• Waist = snatched, sculpted, and defined
• Abdomen looks smoother and more contoured
• Back curves now flow seamlessly into the waist
• Natural shape enhancement — not overdone, just refined
💤 Procedure highlights:
• Performed awake
• No general anesthesia
• No scars, no stitches
• Recovery is typically 4–5 days
#snatched #drsnatched #bodyluxe #FormSculpt #fatremoval
...
Illinois rejected “BBL” on a license plate because it was “too vulgar”… and it had to be explained. 💀🚗
We get it.
At BodyLuxe, BBLs are approved and explained the right way. Our Awake Gold Coast BBL™ is comfortable and safer than general anesthesia ✅🍑
If you’ve been thinking about it, click the link in Bio to schedule your complimentary consultation and check out our current promo.
Parody/satire edit. Not affiliated with the Illinois Secretary of State. Consultation required. Eligibility varies. Results vary.
#BodyLuxe #BBL #AwakeBBL #CosmeticSurgery #PlasticSurgery #AestheticMedicine #BBLConsult #GlowUp #Confidence
Illinois rejected “BBL” on a license plate because it was “too vulgar”… and it had to be explained. 💀🚗
We get it.
At BodyLuxe, BBLs are approved and explained the right way. Our Awake Gold Coast BBL™ is comfortable and safer than general anesthesia ✅🍑
If you’ve been thinking about it, click the link in Bio to schedule your complimentary consultation and check out our current promo.
Parody/satire edit. Not affiliated with the Illinois Secretary of State. Consultation required. Eligibility varies. Results vary.
#BodyLuxe #BBL #AwakeBBL #CosmeticSurgery #PlasticSurgery #AestheticMedicine #BBLConsult #GlowUp #Confidence
...
Awake, comfortable, and watching Elf 🎄
This is what awake FormSculpt® body contouring looks like at BodyLuxe.
Wishing you a cozy and confident holiday season ✨
Visit BodyLuxe.com for promo!
#BodyLuxe #FormSculpt #AwakeLipo #GoldCoastBBL #Chicago
Awake, comfortable, and watching Elf 🎄
This is what awake FormSculpt® body contouring looks like at BodyLuxe.
Wishing you a cozy and confident holiday season ✨
Visit BodyLuxe.com for promo!
#BodyLuxe #FormSculpt #AwakeLipo #GoldCoastBBL #Chicago
...
We’re launching BodyLuxe Lifestyle Reveal!
If you’re an existing patient and you want to be featured, submit ONE lifestyle “after” photo and we’ll create a transition Reel from your pre‑op photo to your real‑life result.
SUBMIT YOURS:
bodyluxe.com/lifestyle
Link in bio to upload + consent.
(You’ll receive a preview to approve before posting.)
#BodyLuxe #RealPatientResults #ResultsVary #glowup #lifestyle #lipo #chicagoinfluencer
We’re launching BodyLuxe Lifestyle Reveal!
If you’re an existing patient and you want to be featured, submit ONE lifestyle “after” photo and we’ll create a transition Reel from your pre‑op photo to your real‑life result.
SUBMIT YOURS:
bodyluxe.com/lifestyle
Link in bio to upload + consent.
(You’ll receive a preview to approve before posting.)
#BodyLuxe #RealPatientResults #ResultsVary #glowup #lifestyle #lipo #chicagoinfluencer
...
After a long week of changing lives, Dr. Farrugia is officially clocking out 💻✨Laptop closed, vibes on — ready for the holiday week ahead — who else is?🎄🕺
#drsnatched #bodyluxe #fatremoval #bbl #minimallyinvasive
After a long week of changing lives, Dr. Farrugia is officially clocking out 💻✨Laptop closed, vibes on — ready for the holiday week ahead — who else is?🎄🕺
#drsnatched #bodyluxe #fatremoval #bbl #minimallyinvasive
...
When your patient sends a twerking video because she’s that excited about her new BBL and tiny waist… we know we did our job. 😌 🍑
Minimal downtime (usually just 4–5 days) and completely awake during the procedure — and she’s already showing off that curvy, sculpted booty.🔥
We absolutely love getting these fun updates from our patients. Keep them coming.✨
#snatched #drsnatched #bodyluxe #minimallyinvasive #fatremoval #fattransfer #bbl #brazilianbuttlift #FormSculpt #twerkthatass
When your patient sends a twerking video because she’s that excited about her new BBL and tiny waist… we know we did our job. 😌 🍑
Minimal downtime (usually just 4–5 days) and completely awake during the procedure — and she’s already showing off that curvy, sculpted booty.🔥
We absolutely love getting these fun updates from our patients. Keep them coming.✨
#snatched #drsnatched #bodyluxe #minimallyinvasive #fatremoval #fattransfer #bbl #brazilianbuttlift #FormSculpt #twerkthatass
...
✨ Dream curves, delivered. ✨
This beauty had unwanted fat removed from her upper + lower abdomen, waist, and flanks—then sculpted into the round, lifted shape she always wanted with a BBL. 🍑
💎 No stitches. No scars. No repeat treatments.
💎 Awake procedure with minimal downtime (just 4–5 days).
💎 One & done for lasting results.
Snatched waistline ➝ sculpted hips ➝ fuller buttocks.
Her silhouette speaks for itself. 🔥
⤴️ Click the Link in Bio to send us a consultation request
📍John Hancock Tower 875 N Michigan Ave Chicago,IL
☎️ (312) 999-5505
#snatched #drsnatched #bodyluxe #minimallyinvasive #fatremoval #fattransfer #bbl #brazilianbuttlift #skintightening
✨ Dream curves, delivered. ✨
This beauty had unwanted fat removed from her upper + lower abdomen, waist, and flanks—then sculpted into the round, lifted shape she always wanted with a BBL. 🍑
💎 No stitches. No scars. No repeat treatments.
💎 Awake procedure with minimal downtime (just 4–5 days).
💎 One & done for lasting results.
Snatched waistline ➝ sculpted hips ➝ fuller buttocks.
Her silhouette speaks for itself. 🔥
⤴️ Click the Link in Bio to send us a consultation request
📍John Hancock Tower 875 N Michigan Ave Chicago,IL
☎️ (312) 999-5505
#snatched #drsnatched #bodyluxe #minimallyinvasive #fatremoval #fattransfer #bbl #brazilianbuttlift #skintightening
...
✨ Thin skin, meet your match. 👋 Did you know you can restore youthfulness to your hands with your own fat? ✨
As we age, the skin on our hands can become thinner, revealing tendons and veins. With fat transfer, we can gently add back volume using your body’s own natural fat, creating smoother, softer, and more youthful-looking hands.
✅ Minimal downtime
✅ Natural results
✅ Long-lasting improvement
Your hands can look as radiant as you feel—without fillers or implants.
#snatched #drsnatched #bodyluxe #fattransfer #handrejuvenation #youthfulhands
✨ Thin skin, meet your match. 👋 Did you know you can restore youthfulness to your hands with your own fat? ✨
As we age, the skin on our hands can become thinner, revealing tendons and veins. With fat transfer, we can gently add back volume using your body’s own natural fat, creating smoother, softer, and more youthful-looking hands.
✅ Minimal downtime
✅ Natural results
✅ Long-lasting improvement
Your hands can look as radiant as you feel—without fillers or implants.
#snatched #drsnatched #bodyluxe #fattransfer #handrejuvenation #youthfulhands
...
Ready to sculpt on the Magnificent Mile? BodyLuxe specializes in awake, minimally invasive liposuction and natural fat transfer—performed under local anesthesia at our Chicago clinic in the John Hancock Center.
👉 Request your consultation: https://bodyluxe.com
📞 Call / Text: (312) 999-5505
📍 Location: BodyLuxe, John Hancock Center, Chicago, IL
Why BodyLuxe:
Awake procedures under local anesthesia (no general anesthesia)
Minimally invasive approach designed for precision and comfort
Natural‑looking contouring and fat transfer options
Downtown convenience on the Magnificent Mile
Procedures we offer:
Liposuction: abdomen, waist, flanks, thighs, arms, chin
Fat Transfer: breasts, buttocks (BBL), hands
Skin Tightening with Renuvion (J-Plasma)
What to expect:
Private 1:1 consultation with the surgeon to confirm candidacy and goals
Personalized treatment plan reviewed by our clinical team
Clear aftercare guidance and support
Go to https://bodyluxe.com to request your complimentary consultation.
Disclaimers:
This video is for informational purposes only and is not medical advice. Consultation is required to determine candidacy. All procedures carry risks; we’ll review these with you in detail. Individual results vary. Footage may feature a model; not a patient.
#BodyLuxe #Chicago #Liposuction #AwakeLipo #FatTransfer #BBL #BodyContouring #MagnificentMile #JohnHancockCenter
Ready to sculpt on the Magnificent Mile? BodyLuxe specializes in awake, minimally invasive liposuction and natural fat transfer—performed under local anesthesia at our Chicago clinic in the John Hancock Center.
👉 Request your consultation: https://bodyluxe.com
📞 Call / Text: (312) 999-5505
📍 Location: BodyLuxe, John Hancock Center, Chicago, IL
Why BodyLuxe:
Awake procedures under local anesthesia (no general anesthesia)
Minimally invasive approach designed for precision and comfort
Natural‑looking contouring and fat transfer options
Downtown convenience on the Magnificent Mile
Procedures we offer:
Liposuction: abdomen, waist, flanks, thighs, arms, chin
Fat Transfer: breasts, buttocks (BBL), hands
Skin Tightening with Renuvion (J-Plasma)
What to expect:
Private 1:1 consultation with the surgeon to confirm candidacy and goals
Personalized treatment plan reviewed by our clinical team
Clear aftercare guidance and support
Go to https://bodyluxe.com to request your complimentary consultation.
Disclaimers:
This video is for informational purposes only and is not medical advice. Consultation is required to determine candidacy. All procedures carry risks; we’ll review these with you in detail. Individual results vary. Footage may feature a model; not a patient.
#BodyLuxe #Chicago #Liposuction #AwakeLipo #FatTransfer #BBL #BodyContouring #MagnificentMile #JohnHancockCenter
...
Snatched for Summer — Jawline Edition ✨
Sculpt a sleek, defined jawline with FormSculpt™ Chin Liposuction + Renuvion® skin tightening — performed awake under local anesthesia at BodyLuxe.
Summer 2025 Special: up to $4,000 OFF select procedures.
Spots are limited—lock yours in now.
Why patients choose BodyLuxe:
✅ Target submental (under‑chin) fat for definition
✅ Renuvion® to tighten & smooth the skin
✅ Awake procedure • Tiny entry points • Minimal downtime*
✅ Performed by Dr. Daniel J. Farrugia in our Chicago clinic on Michigan Avenue
Other Summer favorites: FormSculpt™ fat removal • BBL • Fat transfer to breasts • Skin‑tightening enhancements.
Book your FREE consultation:
🌐 BodyLuxe.com (links in bio)
📞 (312) 999‑5505
📍 John Hancock Center on the Magnificent Mile, Chicago
Financing: 0% for 24 months for eligible clients.
Deadline: Offers valid for procedures performed by September 30, 2025.
—
Medical & offer notes: Results and recovery vary. Not a weight‑loss treatment. Candidacy, areas, and pricing determined at consultation. Financing on approved credit. Renuvion® treats appropriate skin laxity; individual outcomes differ.
#BodyLuxe #FormSculpt #ChinLipo #Jawline #Renuvion #AwakeLipo #SkinTightening #ChicagoAesthetics #HancockTower #Summer2025 #MagnificentMile #Chicago
Snatched for Summer — Jawline Edition ✨
Sculpt a sleek, defined jawline with FormSculpt™ Chin Liposuction + Renuvion® skin tightening — performed awake under local anesthesia at BodyLuxe.
Summer 2025 Special: up to $4,000 OFF select procedures.
Spots are limited—lock yours in now.
Why patients choose BodyLuxe:
✅ Target submental (under‑chin) fat for definition
✅ Renuvion® to tighten & smooth the skin
✅ Awake procedure • Tiny entry points • Minimal downtime*
✅ Performed by Dr. Daniel J. Farrugia in our Chicago clinic on Michigan Avenue
Other Summer favorites: FormSculpt™ fat removal • BBL • Fat transfer to breasts • Skin‑tightening enhancements.
Book your FREE consultation:
🌐 BodyLuxe.com (links in bio)
📞 (312) 999‑5505
📍 John Hancock Center on the Magnificent Mile, Chicago
Financing: 0% for 24 months for eligible clients.
Deadline: Offers valid for procedures performed by September 30, 2025.
—
Medical & offer notes: Results and recovery vary. Not a weight‑loss treatment. Candidacy, areas, and pricing determined at consultation. Financing on approved credit. Renuvion® treats appropriate skin laxity; individual outcomes differ.
#BodyLuxe #FormSculpt #ChinLipo #Jawline #Renuvion #AwakeLipo #SkinTightening #ChicagoAesthetics #HancockTower #Summer2025 #MagnificentMile #Chicago
...
A snatched jawline is just 30 minutes away ⏱️
Tired of that double chin lingering in photos? 📸 This stunning transformation is all thanks to chin fat removal + Renuvion® skin tightening, performed awake and in-office by Dr. Farrugia.
✅ No general anesthesia
✅ Quick recovery—most are back to work the next day
✅ Noticeable definition and tighter skin
From full to flawless in under an hour. This isn’t just about removing fat—it’s about revealing your natural structure and delivering that snatched jawline you’ve been dreaming of. 💫
✨ Sculpted. Sleek. Snatched.
⤴️ Click the Link in Bio to send us a consultation request
📍John Hancock Tower 875 N Michigan Ave Chicago,IL
☎️ (312) 999-5505
#snatched #drsnatched #bodyluxe #snatchedjawline #chinlipo #renuvion
A snatched jawline is just 30 minutes away ⏱️
Tired of that double chin lingering in photos? 📸 This stunning transformation is all thanks to chin fat removal + Renuvion® skin tightening, performed awake and in-office by Dr. Farrugia.
✅ No general anesthesia
✅ Quick recovery—most are back to work the next day
✅ Noticeable definition and tighter skin
From full to flawless in under an hour. This isn’t just about removing fat—it’s about revealing your natural structure and delivering that snatched jawline you’ve been dreaming of. 💫
✨ Sculpted. Sleek. Snatched.
⤴️ Click the Link in Bio to send us a consultation request
📍John Hancock Tower 875 N Michigan Ave Chicago,IL
☎️ (312) 999-5505
#snatched #drsnatched #bodyluxe #snatchedjawline #chinlipo #renuvion
...
This is your season to refine, sculpt, and elevate your confidence.
This limited-time offer ends April 15, and appointments are filling quickly.
Tap below to reserve your consultation and let BodyLuxe sculpt your summer look.